This Post is PG-13: Lovebirds Only
Lo(v)er-ing the barrier to access therapy for sexual dysfunction and intimacy issues
This week’s post for The Innovation Armory is about digitizing therapy options to treat sexual dysfunction and enhance partners’ sexual intimacy. Ok wow, I never thought I’d write a 15 page technology piece on sex! Thanks to Jas Bagniewski, CEO & Co-Founder of Lover, for sharing your perspectives for this piece. Read on for more about:
Why digital sexual therapy is an under-penetrated market (pun intended but regretted)
Benchmarking the sex therapist sector’s supply / demand imbalance vs. other care specialties in the US
Why sexual therapy will benefit from the continued verticalization of digital health platforms
How sex therapy is better suited for online distribution relative to other areas of digital healthcare
Why I use pears, erectile dysfunction, windex, laptop chargers and cappuccinos all in one argument to prove my point
How Lover is building a consumer category leader as the first mover in the digital sexual therapy space
Understanding and predicting the stigmatization curve when analyzing trends as a healthcare tech investor / entrepreneur
How positive psychology should frame our understanding of sex therapy and its commercial potential
Whether we will ever share data on our sex life with dating app companies?
This is a long post so if your email gets clipped at the bottom, make sure to click unclip / visit The Innovation Armory to check out the full read.
If you liked this piece feel free to subscribe for future updates below:
Or share with your friends below :)
Sexual Health is an Under-penetrated Market
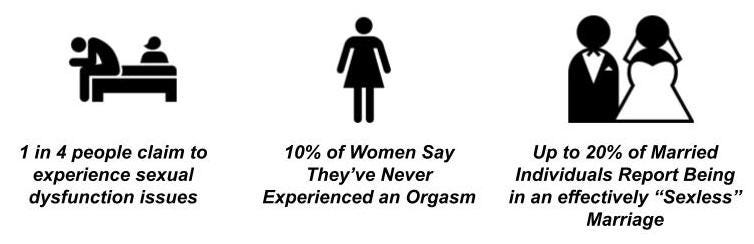
“Sex sells" has been a cliche in the advertising world basically ever since the origins of the marketing industry. New technology tools aimed at improving sexual wellness for couples and individuals seeking to improve the quality of their romantic interactions is giving a whole new meaning to the phrase. Traditionally, sex therapists have dealt with a variety of personal and couples related issues including sexual anxiety, partner communication issues, problems maintaining arousal, physical challenges (such as erectile dysfunction (ED), premature ejaculation (PE), etc.). Most people don’t like to speak publicly about their sex lives - it is taboo, unattractive, embarrassing. But, sexual dysfunction, dissatisfaction and romantic issues are much more common than most people think:
The 25% claiming to experience sexual dysfunction equates to 65 million people in the US alone (25% x 260 million people 18+ in US). This is a conservative estimate as other studies indicate 30-40%. That’s a large market for healthcare services!
While sex therapy may not be the right treatment for this full cohort, there is still a massive assymetry between demand (level of sexual dissatisfaction or dysfunction) and the number of certified sex therapists in the US, which sits at ~1,000 licensed sex therapists in the US today! Let’s say illustratively that only 30% of those with sexual dysfunction in the US are i) sexually active enough and ii) unhappy enough with the issue to ever seek out a sex therapist. That still equates to 19,500 potential patients per certified sex therapist in the US. If you give credit for the full 65 million, this figure is 65,000 potential patients per licensed therapist. This is incredibly high when you compare to broader healthcare metrics for general practitioners / family medicine (118K vs. an 18+ population of 260 million), general pediatrics (61K vs. a <18 population of 73 million) and psychology / psychiatry (106K and 49K respectively for the whole US population).
The relative lack of supply of doctors / patients is 30x greater in sex therapy relative to general practice doctor supply and 220x greater relative to psychology / mental health therapists. There is also reason to believe that the average traditional sex therapist can handle lower caseload than other practice areas. While estimates vary, industry sources indicate the average GP can handle seeing anywhere from 1,500-3,000 patients per year. Mental health psychology caseload is understandably meaningfully lower because psychologists see many patients every week or bi-weekly, each session generally takes 1 hour plus and care situations are infinitely more complex because they aren’t as simple as a formulaic scientific diagnosis and involve one’s partner. Because sex therapy integrates physical, mental and social health issues, there is reason to believe average caseload is closer to psychology but falls somewhere in between the psychology and GP ranges. Not to mention, this supply / demand imbalance is further compounded by geographic differences, as these 1,000 licensed sex therapists are not evenly distributed across the US. This creates a unique opportunity to address this gap with digital products and tele-therapy aimed specifically at the sexual dysfunction and sexual wellness vertical. The supply / demand imbalance validates the volume-based need for more services to meet these healthcare needs. Market size is also determined by price and willingness to pay for healthcare services. I don’t think sex therapy has a willingness to pay issue, but rather an accessibility and stigmatization issue (as will be discussed below). Sexual wellness is pretty critical to the human condition, as illustrated by Maslow’s hierarchy of needs 🙃
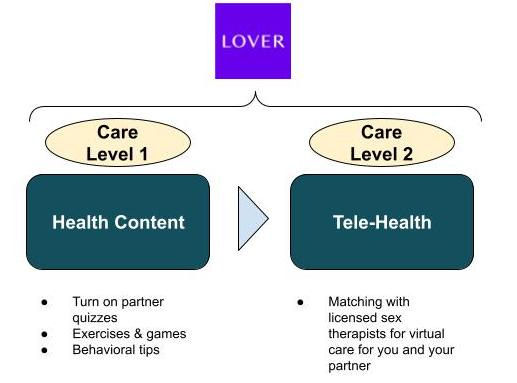
Verticalization of Digital Health
The number of digital health options has exploded as more patients appreciate the cost effectiveness, discreteness and convenience of digital health platforms. For certain health conditions and practice areas, digital health tools are merely part of a multi-tiered escalatory path that may eventually lead to treatment by a traditional practice. This step-care model can start simple with health content, scaling in care complexity to live chat with doctors, tele-health and all the way through to traditional medicine. Digitally-integrated healthcare ecosystems generally have 3-4 different escalation tiers that scale linearly on vectors of convenience, privacy and cost: health content, remote chat, tele-health (video conference) and traditional medicine.
Just as traditional medicine has always been splintered into practice areas where doctors focus on particular verticals, we are starting to see the digital health sphere verticalize into particular practice areas: For example, Apostrophe is teletherapy focused specifically on dermatology and DotCom is focused on pediatric teletherapy. More broadly, tele-therapy for general physical and mental health use cases are segmented between platforms.
I believe the sexual wellness therapy market will benefit from the continued verticalization of digital health platforms. Sexual dysfunction and intimate connection are areas of health that are better suited for digital treatment than traditional care models for more of the population relative to other sectors of medicine:
Privacy & Content Habits - sexual dysfunction (personally or related to intimacy with a partner) is an incredibly sensitive issue to talk about or share with another person. People are naturally inclined to want to deal with those issues on their own / with their partner and not bring in unnecessary outside parties. Unfortunately, because people don’t want to seek help for these issues professionally, they often resort to anonymous community advice on sites like Reddit, which is a pretty ineffective and non-compassionate way of finding solutions to your incredibly personal and meaningful problems. It is very abnormally prevalent for people to privately search sexual problems to seek advice discretely relative to the number of patients that seek help with a licensed sex therapist. I pulled together the below relative comparison of search term popularity between erectile dysfunction and a bunch of common items that you would expect people to search more than ED (pears, windex, cappuccino and laptop charger). Only cappuccino just barely beat out ED.
Plz email me if you think I could have minted an NFT collection out of this incredibly unique search term combination at the top of the last bull market. Please also include what your bid price would have been 🙃
With the level of non-professional content clearly being sought out online related to sexual dysfunction, professional content and tele-health services are likely preferable to many potential patients relative to in-person care. Relative keyword search popularity is just one proxy that demonstrates this opportunity.
Relative Personalization Importance - Lots of traditional tele-health for general practitioners involves screening for a fairly cookie cutter list of symptoms: stuffy nose, headache, etc. whereas, sex therapy does treat issues with physical manifestations but also involves complex relationship dynamics, emotional history and uncovering of prior trauma. This complexity makes personalization even more important so that content and treatment actually better addresses underlying problems. Digital formats that can tap into infinite content libraries and use AI to match patients with sub-care specialists are inherently better at delivering more personalized care experiences
Unit of Treatment - A majority of patients that seek out sex therapy today are in couples or are seeking help to address issues that manifest with their partner. It can make a lot of sense to actively involve your partner in the treatment process if issues stem from relational intimacy. It is logistically easier to schedule recurring appointments and see through joint appointments online when you are planning around two people. Moreover, couples can go through therapy / a plan together, but be served tailored content and have personalized experiences that address their specific issues in the relationship.
Lover is an application that helps individuals and couples discretely address sexual issues (like erectile dysfunction), intimacy issues, but also positively explore turn-ons and learn content to actively improve sexual chemistry with your partner. The initial application is educational content focused and uses the evidence-based sex therapy research of Dr. Britney Blair. They have already seen self-reported improvements in erectile dysfunction comparable to the use of pharmaceuticals like viagra for early users. While the application is initially addressing sex therapy with discrete personalized content, quizzes, behavioral guides and more, over time Lover can offer tele-therapy options to deliver care options across the full spectrum of digital sexual health.
Because of this dual-pronged content and tele-health approach long-term, Lover will benefit from the ability for tele-health sex therapists to leverage its games, content, exercises, etc. as prescription tools to improve outcomes for virtual patients.
I caught up with the Jas Bagniewski (CEO & Co-Founder of Lover) and Dr. Britney Blair (Chief Science Officer & Co-Founder of Lover), to learn more about their vision of transforming sexual wellness and their strong clinical results to-date:
A snapshot from my conversation with Jas below:
“My founders and I were initially drawn to the subject of sex therapy in a startup by the taboo associated with the category. Over 1 in 4 adults have a sexual dysfunction making sexual health the second largest area of mental health in the US after substance abuse disorders, while at the same time there are only 1,000 licensed sex therapists in the whole of the US. Some states like Missouri don’t have any. That combined with the effectiveness of treatment outcomes in sex therapy were really interesting to us. To give you an example, of the 10% of women who have never had an orgasm, 92% can learn simply by being guided through written masturbation exercises by a therapist. And there are similar stats around the efficacy of Cognitive behavioural therapy for conditions like Erectile Dysfunction or low libido. And we see these played out in the efficacy of our product where we see quite dramatic improvements in the sexual health of our users in relatively short timeframes (under a month). Our vision has been to create a private, scaleable and evidence based solution, combined with light touch human interaction to improve the sexual health of our users."
A snapshot from my conversation with Dr. Britney Blair below:
“At Lover, we are taking a scientific and clinical approach to sexual health which is why we went after FDA approval for a more accessible digital product. We are applying this lens to a large problem in intimate relationships and wellness. In fact, sexual disconnect is cited as a top 3 reason for divorce. When sex is going well it constitutes ~20% of the connection in the average relationship but it accounts for ~80% of the disconnect when it’s not going well. Our initial results have been strong in helping bridge the care gap that exists today in this care category. 87% of our users in-app report improvements in and significant decreases in sexual distress after only 2-3 weeks.”
Front-Running the Stigmatization Curve
Mental healthcare was stigmatized for an incredibly long time in the US and is still stigmatized in many parts of the world. For a while in this country, those with now standard mental issues treatable through therapy, medicine, etc. were labeled as “crazy”, “dangerous” and “incompetent”. There are different reasons that a form of care can be stigmatized, but I generally believe there are four different phases that are important to overcome to eliminate stigmatization:
Early on in a potential new treatment area, there is skepticism that i) the issue is actually scientific in nature / mandates care and ii) that there are medically viable treatments with a novel technological method. Hypnotherapy is an example of one current practice area that I’d put in this bucket, which also suffers a branding problem as it is bucketed by most consumers as an entertainment act in a magic show rather than a tool of medicine. Mindset Health is one company that is seeing some traction with its evidence-based approach to hypnotherapy. Once a treatment is taken seriously enough to have societal appeal, various interest groups impose their values onto care options that can create geographic, legal and communal constraints to adoption. Gender-affirming care is a good example where there certain are parts of the country that want to restrict access to care for religious and values-based reasons. I’d frame this value-based hurdle as a negative constraint that drives stigmatization. Once this is overcome, some medical care movements experience branding misalignment, e.g. they are missing positive enabling branding that helps uncertain patients actually take the plunge to seek care. Palliative and hospice care is an area where there is a branding issue about what treatment actually entails, as it encompasses care for life-limiting illnesses and is not just related to immediate end of life / deathbed care. Once all of these constraints are overcome in the national dialogue, stigmas can still persist locally due to differences in distribution and misalignment in access. Mental healthcare used to suffer much more from this problem, which has been alleviated by the rise of tele-therapy platforms.
Sex therapy straddles these three stigmatization barriers: i) certain demographic cohorts stigmatize sex for pleasure pre-marriage, ii) many potential patients don’t fully understand the benefits of sex therapy and iii) there’s an undersupply of therapists across the US. This one goes out to the Harry Potter fans:
A digital platform has the potential to solve all of these simultaneously by using compassionate content and delivering verifiable, personalized outcomes to improve the branding of sex therapy as a category of care, gaining legal approval (Lover already has from the FDA) all while leveraging the low-to-no marginal cost infrastructure of internet care delivery. In the same way that psychology has exploded as a profession and mental health technology platforms have exploded in the wake of this stigma shrinking in mental healthcare, I believe sex therapy has the potential to explode in popularity after crossing the “stigma inflection point”. While this point varies depending on the kind of care, there is an inflection point after which new experimental / younger fields of medicine activate a virtuous cycle for global care needs that beget more talent (doctors) in the field and more patients feeling comfortable seeking care because enough of their network does.
As a first mover in the space, Lover has the unique opportunity of being able to leverage its platform as a positive force to push the entire industry forward across the stigma inflection point to rapidly increase the number of sexual wellness patients willing to seek treatment via digital therapy.
Relative to psychology and mental health therapy, the declining stigma evolution here will be different. Mental health therapy crossed the stigma inflection point through the use of real world distribution of psychology services and then digital options followed subsequently. A large portion of the market in tele-therapy consisted of the care gap between traditional therapy supply and demand. In the case of sex therapy, the market is not just this care gap, but rather platforms like Lover are helping to more actively define and shape the market from the ground up. We need apps like Lover for sex therapy to cross stigma inflection and we may not cross it first with just real world therapy options. Because of this unique dynamic, digital sexual wellness therapy can supersede offline therapy as the primary form of care in a way that may not be possible in other fields of medicine. This is akin to how Headspace and Calm have taken over meditation therapy, as digital platform usage in these verticals is much more prevalent than in-person meditation coaches.
Changing The Conversation on Care
After mental healthcare crossed the stigma inflection point, a new area of psychology began to gain in prominence called positive psychology, a term coined by Martin Seligman. It distinguishes negative (traditional) and positive psychology. Traditionally, patients see psychologists to address specific psychological problems they are having, which assumes the patient has some pre-existing issue to work through. Positive psychology seeks to use psychological methods to enhance life for those who are already overall healthy rather than seeking to restore or repair illness in negative care patients.
The positive psychology analogy is highly relevant to the conversation of sexual therapy and care. Most sex therapists today seek to address sexual dysfunction and romantic intimacy issues, rather than using therapy as a means to improve and enhance an already healthy sexual chemistry between partners. Lover is doing both with its platform and is helping expand the use case further for the latter.
The positive care use case is much more aligned with digital content as the distribution engine as it relates more to education and discovery rather than addressing an issue. This understanding of sex therapy catalyzed by a digital platform like Lover is transformative to market size by establishing a broader use case that makes the market more relevant for all sexually active adults as opposed to just sexually dysfunctionally adults. This approach is more likely to win out in the consumer landscape because the negative therapy side of the business can serve as a lead generation engine to get users onto Lover’s app and the positive therapy side of the business is for customer retention and upsell once users improve their core set of sexual and intimacy problems.
Besides the ability to move users from negative therapy into positive therapy, relative to other kinds of treatment, sex therapy patients are more likely to recur than other types of individual therapy because many of the issues are relational and contextual. An individual may have different sexual chemistry and intimacy issues to address with different partners. Therefore, as younger users go through the dating pool, they are more likely to continue a subscription to leverage different content and programs that may be more applicable with different types partners over time.
While many adults experience sexual dysfunction and intimacy issues, reports indicate that up to 90% of them go untreated. By normalizing the discussion around sexual health, opening up a discrete treatment avenue and shifting the conversation to emphasize positive therapy, Lover is the type of business that can catalyze a meaningful expansion of its own addressable market by encouraging more untreated patients to seek care. Once this treatment hesitancy barrier is broken, given the personal and intimate nature of this kind of care, I would suspect user loyalty has the potential to be even higher here relative to other digital health products.
A broader macro issue at play that is impacting the discourse on sex therapy is the impact of school sex education (or lack thereof) into adulthood. Legislation for sex education is a states rights issue and while 50% of states have legislation mandating sex education, only 13 states require it to be medically accurate with many being i) not sexual orientation inclusive and ii) many stressing or educating expressly about abstinence. The below chart from Guttmacher Institute summarizes the deficiencies across states and the impact of values differences on sex education across the US:
Even in states where there is sex education, these programs are in no way personalized and don’t equip young adults with the knowledge and tools to understand their full development path as their sexual identity changes into adulthood. Over time, platforms like Lover will play a critical role in educating young adults about their own sexual development in states where sex education is non-existent or otherwise wholly deficient.
Swiping Between the Sheets
Over time, dating apps have grown across the world in popularity as one of the preferred means of dating. The US leads the world in dating app penetration at 15.7% of its population:
Swiping on profiles can provide a preliminary proxy on a lot of the key attributes people care about when dating, but there’s one it can’t quite nail down. Can you guess which?
While most dating apps can gauge potential match quality through common interests, photos, chat and profile prompts, none of these inputs help partners gauge potential sexual chemistry with one another. It’s interesting to consider whether Lover could work with dating apps to allow users to consent to share results from certain assignments, games and quizzes from their positive sex therapy as a means of improving match quality by screening for mutual sexual compatability and chemistry. This would purely be for the dating algorithms to better choose which profiles to present to swipe on, not for any of this information to actually be displayed in profiles. There could be some HIPAA issues to work through here as a digital health platform, but if users own their own data, then they could choose to share it with another application if it meaningfully enhances their online dating experience. This is definitely one of those ideas that our grandparents would look back on as utterly ridiculous and an unnecessary push towards hyper-efficiency:
All Innovation Armory publications and the views and opinions expressed at, or through, this site belong solely to the blog owner and his guests and do not represent those of people, employers, institutions or organizations that the owner may or may not be associated with in a professional or personal capacity. All liability with respect to the actions taken or not taken based on the contents of this site are hereby expressly disclaimed. These publications are the blog owners’ personal opinions and are not meant to be relied upon as a basis for investment decisions.